▼▼▼
wowbonus

Бонус 7000 рублей от Мелбет за регистрацию
Букмекерская компания мелбет, как и многие другие операторы, предлагают своим игрокам различные бонусы. На сегодняшний день бонусная программа на официальном сайте букмекерской компании значительно расширилась и пользователям доступные разны виды привилегий и поощрений. Важно отметить, что для получения любого из доступных бонусов, важно выполнить условия, которые также прописаны и находятся в общем доступе.

Как получить бонус в melbet?!
Учитывая тот момент, что поощрения бывают разными, условия также могут серьезно отличаться.
В большинстве своем, для получения бонуса приходится пройти полный процесс регистрации на официальном сайте bk, с учетом идентификации.
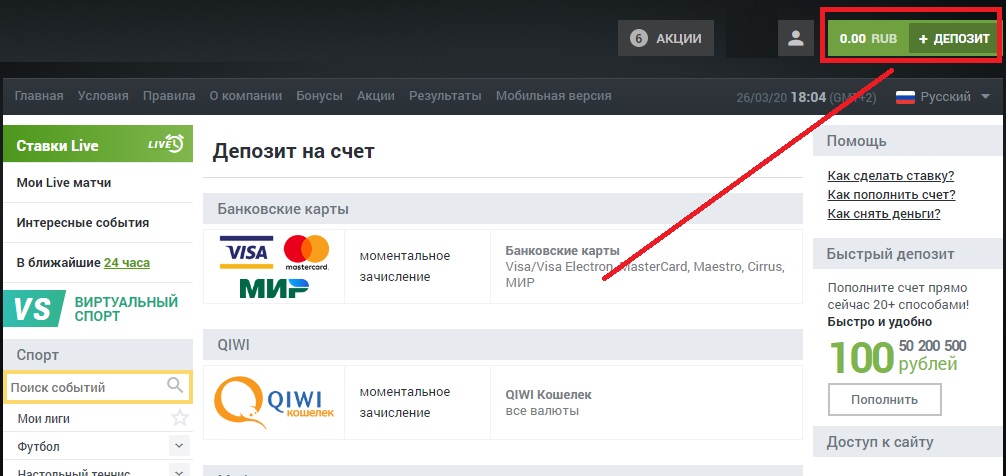
В отдельных случаях нужно внести первый депозит, или же вписать промокод для получения бонуса.
Более того, в отдельных видах бонуса, после зачисления средств на специальный счет, нужно пройти еще и процесс отыгрыша. Лишь после этого полученные средства становятся доступными для дальнейшего использования. Больше узнать о том, как отыграть бонус в мелбет можно на сайте БК.
Бонус за регистрацию
Такой тип поощрения подразумевает предоставление бонусных средств за простую регистрацию на сайте букмекерской компании. Бонусы при регистрации в melbet периодически появляются и искать их нужно в разделе с акциями.

100% на первый депозит
Абсолютно все новые пользователи, которые решатся внести первый депозит после регистрации на сайте, имеют возможность получить еще 100% от внесенных средств в виде бонуса. Минимальная сумма пополнения баланса – 100 рублей. Следовательно, пользователь, который внесет эту сумму, уже может получить определенную привилегию.
Страница бонуса на 1-вый депозит
Этот бонус – это как раз-таки тот случай, когда его нужно отыграть. То есть, перед тем как вывести бонусные деньги с мелбет, нужно проследовать четко обозначенной процедуре.
Последовательность действий такова:
- Нужно проставить сумму в 5-кратном размере от внесенного депозита;
- Делать это нужно, заключая пари типа “экспресс”;
- В каждом купоне должно быть не меньше 3-х событий;
- Минимальный коэффициент позиции – 1.40.
Если пользователю удается выполнить эти условия, он автоматически становится обладателем этих средств и может вывести их на реальный счет, и спокойно использовать, делая ставки в melbets, либо выведя их на карту.
Фрибеты в БК melbet
Букмекерская компания мелбет предлагает фрибет, кратный 100% от суммы внесенного депозита. То есть, это тот же бонус на первый депозит, о котором ранее и шла речь.
Но тут система отличается. Игроку необходимо:
- Поставить весь депозит на событие с коэффициентом 1.5;
- В случае выигрыша получить фрибет, раный сумме депозита;
- Проставить фррибет трижды на любое событие с коэффициентом 1.4.
Периодически на сайте появляются и другие предложения с бонусными фрибетами, для этого нужно регулярно проверять раздел с бонусами и акциями, который расположен на официальном сайте букмекерской компании.
Подробные правила по фрибету
Промокод в букмекерской компании Melbet
Сейчас на сайте есть сразу несколько актуальных промокодов, которыми могут воспользоваться новички.
При создании аккаунта можно также указать наш фирменный промо-код, увеличивающий сумму максимального бонуса на 30%:

После вводу указанного кода – появляется уведомление
Чтобы отыграть полученный бонус, нужно проставить его в том же 5-кратном размере, составляя экспрессы, состоящие из 4-х событий и более.
Минимальный коэффициент, который будет браться в учет – это 1.40.
Как минимум 3 позиции в экспрессе должны быть с таким коэффициентом, остальные по желанию.
Перед тем как использовать бонус в мелбет, следует подробно ознакомиться со всеми условиями. Вся информация о бонусах в мелбет 365 есть на официальном сайте букмекерской компании.
Акции в букмекерской конторе
Это особый раздел привилегий, куда включены различные розыгрыши призов и другие интересные предложения. Здесь также есть перечень условий, получить деньги можно лишь в случае, если вы окажетесь в числе счастливчиков.
Раздел акций и бонусов
Обычно, участие в акциях подразумевает выполнение условий, внесение взносов и другие действия.
К примеру, сейчас можно выделить такие актуальные предложения, как:
- 100% возврат. Акция подразумевает составление игроком экспресс ставки, в котором должно быть минимум 3 события с коэффициепнтом 1,7. Если одно из событий не играет – букмекер возвращает сумму ставки;
- Подарок на день рождения. Букмкеер может подарить клиенту бесплатные попытки игр (фриспины) для раздела азартных развлечений в честь дня рождения;
- Экспресс дня. Повышенный коэффициент на предложенный букмекером купон.
Также на сайте функцонирует программа лояльности. Периодически, на сайте melbet появляются и другие интересные предложения. Регулярно пополняя счет, выводя деньги и заключая пари, можно принимать участие в разных акциях. Единственное, что важно понимать – это как вывести бонусные деньги с мелбет и как их использовать.
На сайте вся эта информация доступна и ее нужно только найти.
Бонусная программа от БК Melbet Как и другие букмекеры Мелбет в маркетинговых целях активно продвигает свои собственные бонусы и акции. Следует отметить, что бонусная программа распространяется на все категории клиентов, как на новичков, так и на бетторов со стажем. Самое первое, что ждет игрока в момент регистрации в Melbet — выбор бонуса. Для новичков, которые впервые регистрируются в качестве клиентов букмекера, самым щедрым предложением является приветственный бонус.:
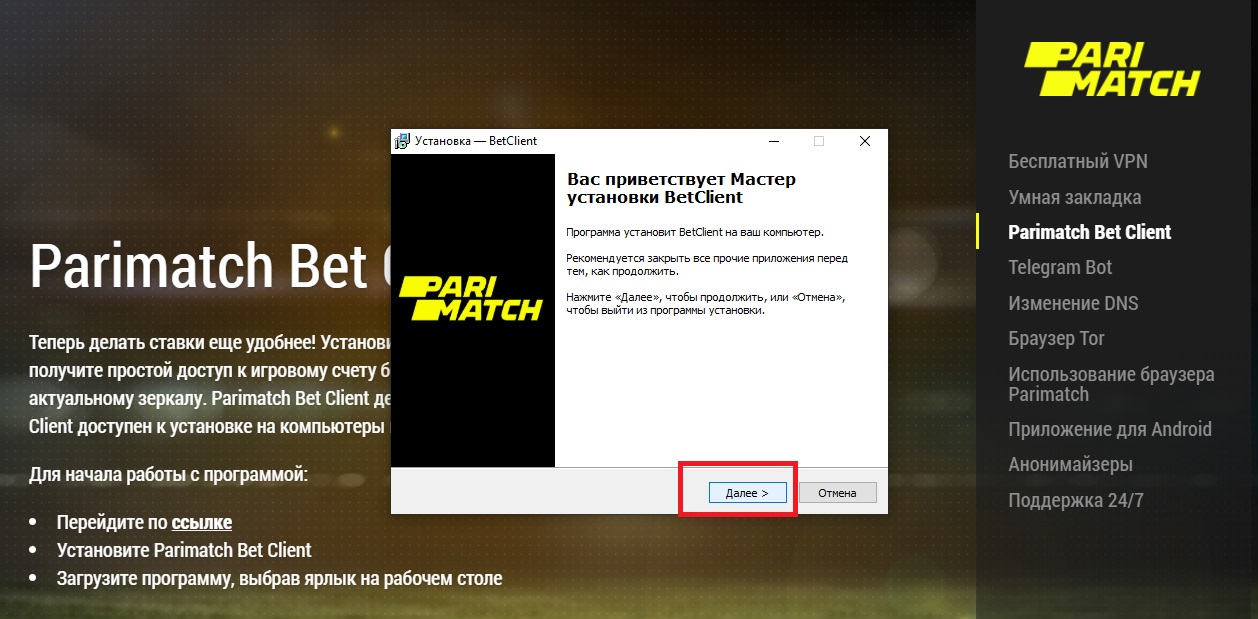
- мелбет зеркало сайта
- рабочая ссылка мелбет
- melbet host
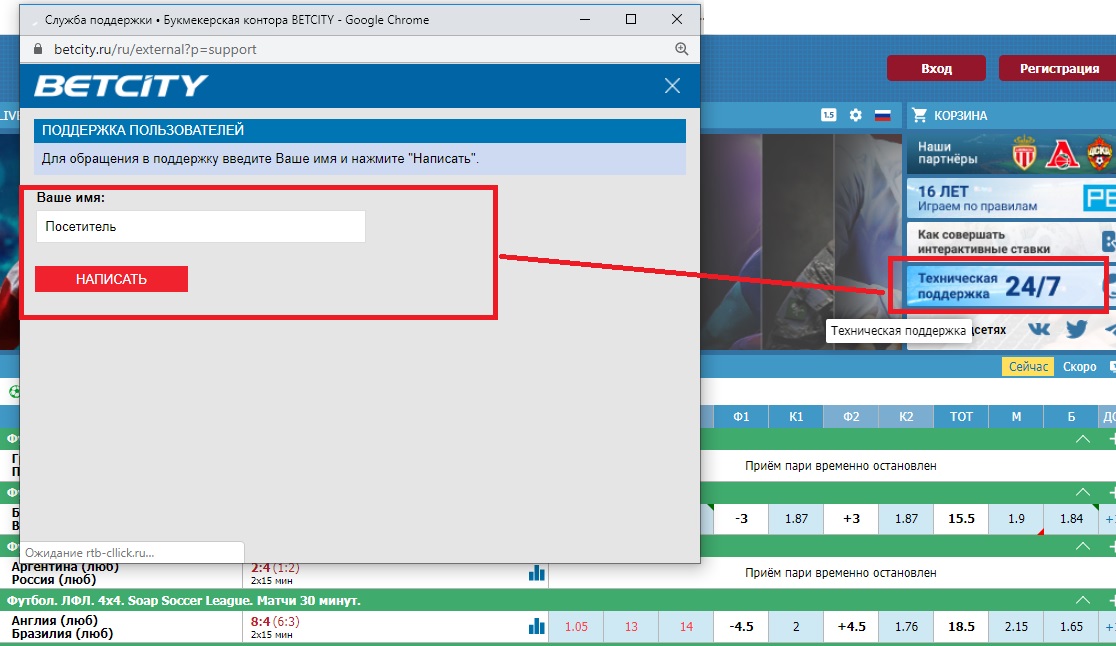
- мелбет контакты
- мелбет ютуб

